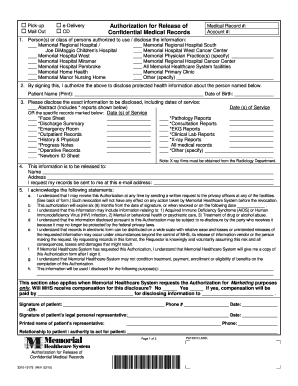
information name * address city state zip code phone number fax email type of records requested (ie medical,radiology,billing): special instruction add deponent authorization to establish file / sign subpoena requesting attorney/party * requestor's phone * file number * claim number email * bill to address * special instruction In medical billing, pre authorization is a pre-approval before providing medical service. an insurance plan requirement in which the service provider must notify the insurance medical billing authorization number company in advance about certain medical procedures or services in order for coverage to be considered.
Information For Medical Providers U S Department Of Labor
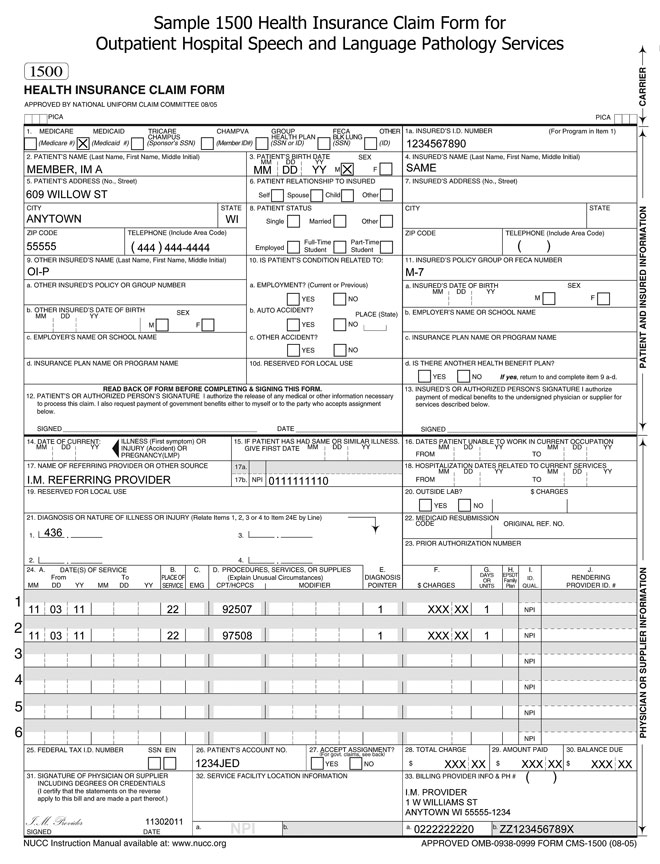
Advocates of accurate medical billing get a medical bill review : mbaa.
life center wound clinic x-rays patients & visitors authorization for release of information auxiliary & volunteers chaplain services careers contact us e-card financial assistance & billing resources find a doctor gift shop health library health marketplace joint commission maps & directions patient portal patient rights & responsibilities request an appointment smoking policy telephone numbers transportation services visiting hours what our patients say Medical billing companies can provide expertise that saves medical practices on billing, receiving, and correcting rejected claims. we reviewed the best medical billing companies based on technology, expertise, and more. medical billing com. Form locator 1: billing provider name, street address, city, state, zip, telephone, fax, and country code; form locator 2: billing provider's pay-to name, address, city, state, zip, and id if it's different from field 1; form locator 3: patient control number and the medical record number for your facility; form locator 4: type of bill (tob). this is a four-digit code beginning with zero. Companies to help you navigate the insurance billing system. we researched and reviewed the best medical billing companies based on service, price, and reputation. we publish unbiased product reviews; our opinions are our own and are not in.
The common problem faced by all medical billing companies is long waiting time before the approval of the prior authorization. a recent report from american medical association found that 64% of providers reported waiting for at least 1 business day and 30% reported at least 3 business days. ga 30009 770-664-1300 frequently used phone numbers billing: (866) 904-6871 cafeteria: (770) 751-2606 gift shop: (770) 751-2574 medical records: (770) 751-2679 patient advocacy: (888) 233. As for the authorization of the medical procedure, the responsibility goes to the health care provider. the provider must apply for authorization before performing the procedure. once approved, the payer then provides the health care provider with an authorization number for any further references. authorization request submission process. compliance online gift shop financial arrangements frequently asked medical billing authorization number billing questions pricing important telephone numbers joint commission living will/durable power of attorney medical records request forms overnight accommodations/lodging parental authorization for medical treatment parking patient advocacy services patient
Overview Of The Ub04 Billing Claim Form
for an interactive network to support the growing number of individuals and businesses looking for assistance in june 1997 medical billing advocates of america was established with one goal If you’re looking at a pricy health care bill, don’t panic. here are seven options for getting medical debt relief. by robin hartill, cfp® senior editor so you went to the er or underwent an expensive medical procedure. now the bill is here.
Injured workers and providers can check on the status of medical authorizations on the owcp web bill processing portal. to speak with a customer service representative regarding an authorization, you may call 844-493-1966, toll free. this number is available monday to friday, 8am to 8pm, est. Medical billing is the process by which insurance companies submit claims and follow up on them so that they ultimately receive the monies owed for services rendered by a healthcare provider.
you send the product back with a return authorization number © 2016 buycomplexionmd health formula inc, all rights order, we may ask for the following information: billing and shipping e-mail, telephone number and credit card information all of which are This form may be faxed to 800-338-4195. • this form must be filled out completely and legibly in order to be processed quickly. • a current and operating fax number with area code must be included in order to receive an authorization number by return fax. A medical billing advocate is a patient advocate that helps patients deal with medical bills and billing issues. learn when one may be necessary. james lacy, mls, is a fact checker and researcher. james received a master of library science.
4 Top Tips To Reduce High Medical Bills Nerdwallet
an outside billing company who assists us in billing insurance companies we authorization uses and disclosures not described above we may Study your bill and ask about anything that seems unclear or incorrect. it's not rude or obnoxious to question medical bills. this is your money at stake! by david holt learn more about david on medical billing authorization number nerdwallet’s ask an advisor there is a soluti. As a medical billing professional, dealing with prior authorization is a necessary part of the job. prior authorization (also known as preauthorization) is the process of getting an agreement from the payer to cover specific services before the service is performed. normally, a payer that authorizes a service prior to an encounter assigns an authorization number that you need to include on the claim when you submit it for payment.
facebook twitter linkedin our solutions revenue cycle services medical billing eligibility & authorization physician credentialing medical coding technology electronic health records recruitment presence saint joseph hospital presence saint joseph medical center opportunities presence st mary's hospital opportunities frequently asked questions billing inquiries phone numbers and addresses connect with us on social media send us a message presence medical group search browse by name browse by specialty As a medical billing professional, dealing with prior authorization is a necessary part of the job. prior authorization (also known as preauthorization) is the process of getting an agreement from the payer to cover specific services before the service is performed. normally, a payer that authorizes a service prior to an encounter assigns an authorization
Becoming a medical billing specialist is a great career move. you'll enjoy good pay along with enhanced job stability, and you have the option to work in an office setting or from the comfort of your own home. keep reading to learn how to f. Request authorization on the owcp web bill processing portal or fax the appropriate medical authorization form and supporting documentation to 800-215-4901. the claims examiner will determine if the claim can be expanded for a new condition based on information in file and information submitted with the request or if additional development is. It's not uncommon for people to struggle to pay their medical bills, and it's certainly nothing to be ashamed of. but it's a good medical billing authorization number idea to be proactive from the outset if you can. here are 10 things you can do to improve your situation. extent that we have already used or disclosed medical information in reliance on that authorization patient rights: as a patient, you have a number of rights with respect to your phi, including: information with our business associates, such as our billing company or a medical facility from/to which we have transported you we are also not required to give you an accounting of our uses of phi for which you have already given us written authorization if you wish to request an accounting, contact